Good nutrition is important in both health and disease. Our body requires approximately 50 different nutrients to function at its best. It obtains these nutrients from the food and beverages we consume.
The proper array of nutrients can be obtained by consuming a balanced diet that includes foods from all the food groups.
- GRAINS: Choose whole grain breads & cereals with fiber.
- VEGETABLES: Choose a variety of colors, especially dark green and orange varieties.
- FRUIT: Choose a variety of colors.
- DAIRY: Strive for 3 cups of milk or yogurt each day.
- PROTEIN: Choose more lean protein choices, such as poultry and fish. Vary your protein intake by choosing nuts, seeds and beans/peas.
- FATS/OILS: Strive to consume heart-healthy fats like olive, canola or peanut oils.
Why is nutrition important for those living with ALS?
- To meet the increase energy needs caused by ALS
- To slow the process of muscle breakdown common with ALS
- To keep the immune system strong and ready to fight infection
- To maximize energy levels
- To improve your sense of well-being and quality of life
Nutrition Difficulties You May Encounter
- Weight Loss
- Poor Appetite
- Swallowing/Chewing Difficulties
- Dehydration
- Constipation
- Fatigue
- Thick Saliva
Energy/Calorie Needs
Maintaining a good nutrition status can be difficult when living with ALS. Decreased appetite, stress and trouble chewing or swallowing can affect your food intake. However, your energy needs are perhaps greater than ever before.
Research is showing the following regarding calorie needs in those with ALS:
- Your energy needs are approximately 15% higher than someone who does not have ALS.
- Inadequate nutrition intake will speed up the break down and weakening of extremity and breathing muscles.
- A large percentage of ALS patients consume fewer calories per day than the amount they require.
- Weight loss and inadequate energy intake may accelerate the progression of the disease.
Recommended Body Weight
Monitoring your body weight is one way to keep an eye on your nutritional status. It is generally recommended that you do not try to lose weight once you are diagnosed with ALS. The goal is weight maintenance. You may experience minor weight loss due to a reduction in muscle mass. However, dieting is not recommended, even if you feel you are overweight.
Make an effort to keep track of your weight.
- Keep a chart of your weight starting today!
- Weigh yourself once a week, preferably the same day and time each week.
- Compare any changes to your usual adult weight, rather than comparing to standardized weight charts.
- Fluctuations of 1-2 pounds are common. However, if you notice a trend of weight loss, be sure to notify your doctor and dietitian.
Loss of Appetite
You may experience a reduction or loss of appetite. It is important even during these times to maintain an adequate energy intake. If you experience a loss of appetite try some of the following:
- Eat well during your “up” times
- Eat smaller, more frequent meals
- Avoid long periods of time when you are not eating
- Be sure to eat nutrient-dense foods rather than light or diet foods
- Eat first and then drink. This will allow your stomach to fill up with foods rather than just liquids
- When you drink, make sure you are drinking beverages that offer calories (milk, juices, egg nog, and nutritional beverages)
- Keep your favorite foods around the house
- Make sure meals are pleasant times. Make the environment comfortable and attractive
- Try a variety of foods of different tastes, textures and temperatures
- Serve food in small portions on small plates
- Make a schedule for eating and follow it like you would for your medicine
- Eat with other people
- Serve foods attractively
- Keep a variety of handy, ready-to eat snacks available
Ways to Increase Your Calorie Intake
If you lose your appetite or begin to lose weight be sure to address the problem early on. Often eating more food is not an option, so you will want to increase the number of calories in the food you do eat. To do so you may have to increase the amount of fat or sugar in your diet. Use the suggestions below to maximize your calorie intake.
- Add fats to your foods. These include
- Butter
- Margarine
- Gravy
- Olive oil
- Mayonnaise
- Cream Cheese
- Sour cream
- Peanut Butter (unless swallowing problems exist)
- Salad dressing
- Nuts (unless chewing/swallowing problems exist)
Add these fats to all kinds of foods: breads, hot cereals, rice, potatoes, vegetables or any other food you enjoy. This will increase your calorie intake without increasing the overall quantity of food you eat.
- Add calories via high sugar condiments
- Jams, jellies
- Marmalade
- Honey
- Maple Syrup, chocolate syrup
- Sprinkle grated cheese on vegetables, casseroles, soups, eggs
- Use dips for your favorite breads, crackers, fruits, and vegetables
- Make things with milk, preferably a higher fat milk (oatmeal, mashed potatoes)
- Add dry milk powder to your regular milk, gravies, sauces, and puddings
- Make hot cocoa, soups, or puddings with half and half or evaporated milk
- Add additional meats or dried beans to your soups and casseroles
- Drink a nutritional supplement each day for added calories and protein.
- Ensure Plus® (350 calories/13 g protein per 8 ounces)
- Boost Plus® (360 calories/14 g protein per 8 ounces, Lactose free/contains milk protein)
- Carnation Instant Breakfast® (220 calories/13 g protein per 8 ounces, contains milk)
- Slim Fast® (approximately 200 calories/10 g protein per 11 ounces)
- Resource 2.0® (480 calories/20 g protein per 8 ounces)
Recipes
Banana Smoothie
Ingredients (Makes: 1 1-cup serving)
1 8-fluid-ounce bottle of Ensure® Original Vanilla
1 small ripe banana
1/4 teaspoon vanilla extract
Directions
In a blender, combine all ingredients. Blend until smooth. Pour into a tall glass and serve.
Per 8 oz serving: 340 calories/10 g protein
Frozen Fudge Pops
Ingredients (Makes: 7 popsicles)
1 cup skim milk
1 cup (8-ounce) Ensure® Original Milk Chocolate
1 3.5-ounce package regular instant chocolate pudding mix
1-1/2 cups lite frozen whipped topping
½ cup chopped (two 1.76-ounce) Zone Perfect® Double Dark Chocolate Bars
½ cup toasted almonds, chopped (omit if swallowing problems)
Paper cup, wooden pop sticks, or frozen pop containers
Directions
In a mixing bowl, whisk together the milk and Ensure®.
Add the pudding mix and continue to whisk for 1 minute.
Fold in the whipped topping, chopped bars, and nuts.
Spoon mixture into molds or paper cups.
Insert wooden sticks or spoons and freeze about 5 to 6 hours or until firm.
Unmold and serve.
Per popsicle: 230 calories/8 g protein
Recipe from www.ensure.com
Chocolate Malt Shake
Ingredients
1 envelope Carnation Chocolate Malt Instant Breakfast®
1-1/2 cups vanilla ice cream
1 cup cold whole milk
Directions
Place all ingredients in blender container.
Cover and process on high speed until well blended.
1 serving (2-2/3 cups): 678 calories/20 g protein
P'Nut Protein Booster
Ingredients
1 envelope Carnation Chocolate or Vanilla Instant Breakfast®
1 cup cold whole milk
2 tsp. wheat germ
2 tsp. peanut butter
Directions
Place all ingredients in blender container.
Cover and process on high speed until well blended.
1 serving (1-1/2 cups): 360 Kcals/ 17 gm Protein
Boost® Oatmeal
Ingredients
1/2 cup Boost® Vanilla
1 package instant oatmeal
Cinnamon or nutmeg to taste
Directions
Pour oatmeal into microwavable bowl.
Stir in Boost®. Mix well.
Microwave, uncovered 1 1/2 - 2 minutes until thickened (bowl will be hot).
Sprinkle with cinnamon and/or nutmeg.
Let stand until desired consistency.
1 serving: 220 calories/8 g protein
Recipe from: www.boost.com
Boost® Custard
Ingredients
1- 2.9 oz. box custard mix
1 - 8 oz. bottle Boost® Vanilla
1 cup milk
Directions
In a small saucepan stir together custard mix, Boost® and milk. For richer custard, add 1 well beaten egg yolk. Stirring constantly, cook on medium heat until mixture comes to full boil. Remove from heat.
Pour into dessert dishes. Sprinkle with nutmeg. Refrigerate for 1 hour or until set.
(Makes 4 - 1/2 cup servings)
Per 1/2 cup serving: 160 calories/6 g protein
Recipe from: www.boost.com
Chewing and Swallowing Difficulties
If the muscles of chewing and swallowing become weak, some changes in your diet may be helpful in order to reduce fatigue and lower your risk of choking. The following tips are guidelines to decrease your risk of aspiration (food going down the wrong pipe). However, be sure to get a referral to a speech/swallowing specialist to determine what consistency of foods and beverages are safest for you.
Keep in mind that not everyone with ALS develops problems with swallowing. You may continue to consume foods and beverages of a regular consistency as long as you have not experienced chewing/swallowing troubles.
Signs and Symptoms of Swallowing Problems
- May experience weakness in tongue, facial and muscles of mastication
- Prolonged mealtimes
- Fatigue with chewing
- Difficulty pushing food back with tongue
- "Sticking sensation" in throat with solid food
- Occasional coughing with thin liquids
- Multiple swallows required to "get food down"
Tips for Safe Swallowing
- Eat in a relaxed environment
- Sit in upright position
- Eat slowly
- Small bites/sips
- Concentrate on swallowing
- Cough when needed to clear food in throat or material which may have entered into airway
- Whenever you cough, swallow immediately before breathing again
- Keep suction machine nearby
- Clean mouth after eating
- Remain in upright position for about 30 minutes after meal
Texture
Foods that are easy to chew and that stick together in the mouth are often recommended when chewing or swallowing problems arise.
- Egg dishes such as soufflés, quiches, omelets
- Custards, puddings
- Egg, tuna or chicken salad with extra mayonnaise
- Gelatin
- Mashed potatoes with gravy or margarine
- Well cooked vegetables without skins
- Meatloaf - very moist, extra gravy
- Soft cheese
- Canned fruits (drained)
- Ripe bananas
- Cooked cereals with milk
- Creamy macaroni and cheese
- Applesauce
You will want to avoid foods that are crumbly, or that fall apart easily in your mouth. Use caution with foods that have tough skins or seeds and with sticky foods.
Examples include:
- Raw fruitss and vegetables
- Nuts
- White bread
- Plain ground meats (those without gravy)
- Dry cereal
- Coconut
- Pineapple
- Peanut butter
- Peas, corn, legumes
- Rice
- Scrambled eggs
- Cornbread, dry muffins
- Crackers
- Popcorn, potato chips
Mixed consistency foods can also be problematic for some individuals. These include foods that contain both a liquid and a solid.
Examples include:
- Chunky soups
- Cold cereal with milk
- Citrus fruits
- Vegetable soups
- Gelatin with fruit
- Salads with dressing
Liquids
If you notice thin liquids (water, tea, juice, and coffee) are slipping down the wrong pipe, try drinking thicker liquids. Thicker liquids resemble the consistency of fruit nectar. They may include milkshakes, eggnog, fruit nectars and yogurt drinks. You may also thicken the thinner liquids by using a home or commercial thickener.
Commercial Thickening Agents
|
Product
|
Manufacturer
|
Phone
|
Web Address
|
|
Thick and Easy®
|
Hormel Health Labs Inc.
|
1-800-866-7757
|
|
|
Resource Thicken Up®
|
Nestle Nutrition
|
1-800-333-3785
|
|
|
Thick-It®
|
Precision Foods, Inc.
|
1-800-333-0003
|
|
|
Simply Thick®
|
Simply Thick
|
1-800-205-7115
|
|
|
Thixx®
|
Bernard Food Industries
|
1-800-323-3663
|
|
Home Thickening Agents
|
Cornstarch
|
Thicken juice by cooking one cup of juice with 1 Tbsp cornstarch
|
|
Arrowroot
|
Thicken fruit juice by cooking one cup juice with 2 tsp arrowroot
|
|
Instant Potato Flakes
|
Add to soups, sauces, gravies or pureed dishes; ¼ c flakes added to 1 cup soup
Can also be used to thicken pureed vegetables.
|
|
Instant Pudding Mix
|
Add to milkshakes, 2-4 Tbsp per 10 oz shake (prepare 30-40 minutes before using shake). Adds 30 calories per Tbsp.
|
|
Instant Rice Cereal
|
Thickens soup or juices. Use 2 Tbsp per ½ cup.
Can also be used to thicken pureed fruits.
|
|
Cheese
|
Add to soups, pureed casseroles or meat. Adds calories and protein in addition to thickening
|
|
Gelatin
|
Can be used to thicken cold liquids.
Use flavored gelatin to help thicken pureed fruits.
|
Some people with ALS need to thin their foods and beverages.
To thin your food add:
- Broth
- Bouillon
- Gravy
- Juice
- Liquid flavored gelatin
- Melted butter or margarine
- Milk
- Plain yogurt
Temperature
Hot or cold foods are generally easier to swallow than luke-warm or room temperature foods. Ice-cold beverages are also easier to swallow than room temperature beverages.
Taste
Keep foods flavorful! Foods with stronger flavors can be easier to swallow than bland foods. Add herbs, seasonings, sugars or citrus juices to your foods for enhanced taste.
Dehydration
Dehydration can be common amongst those with ALS. Lack of appetite or difficulty swallowing may cause people to reduce their fluid intake.
Signs and Symptoms of Dehydration
- Decreased urine output
- Difficulty swallowing
- Dry mouth
- Constipation
- General fatigue
- Low-grade fever
- Thickened mucous/secretions
You should strive to drink at least 8 cups of non-caffeinated fluids everyday to maintain a good hydration status. Try the following to help maximize your fluid intake.
- Keep a beverage with you at all times
- Take a drink from a water fountain when you pass by
- Eat foods with higher water contents such as canned fruits, custards, yogurts and puddings
- Try some frozen juice bars, sherbet or popsicles
- Freeze a bottle of soda and consume it as a slushy.
** If you have been advised to consume thickened liquids you will want to avoid regular ices, popsicles, ice cream and sweetened gelatin desserts as these melt to thin liquids in your mouth. Try preparing your own gelatin dessert with the amount of fruit juice and gelatin that will thicken to the appropriate consistency.
- Constipation
Constipation is common among those living with ALS. This is due to the weakening of the abdominal muscles and a reduction in activity level. Inadequate fluid intake and inadequate fiber in the diet can also contribute to this problem. In turn constipation can cause discomfort and a reduction in one’s appetite.
To help with constipation:
- Walk as much as you are able.
- Ensure adequate fluid intake: 8 glasses of non-caffeinated fluids daily will help soften the stool.
- Start your day with a glass of prune juice or warm water with lemon.
- If you do not have problems with swallowing include high fiber foods in your diet such as whole wheat breads, brown rice, high fiber cereals, beans, vegetables and fruits.
- If you are taking a nutritional supplement, try one with added fiber (for example, TwoCal HN®)
- Try 2 servings each day of ACTIVIA ®Greek yogurt by Dannon Foods.
- Shown to help reduce intestinal transit time
- Visit www.activia.com to learn more
Fatigue
Feeling tired and worn out is a common symptom of ALS. If you feel too tired to eat consider:
- Taking a nap before meals
- Eating soft foods that require less/minimal chewing (i.e.: puddings, ice cream, yogurt, soups, egg and tuna salads, mashed potatoes with gravy and oatmeal)
- Drink a nutritional supplement as part of or for all of a meal. Discuss with a registered dietitian what supplement and how much of a supplement would be appropriate to use for a meal replacement
- Try eating 6 small meals per day instead of 3 larger meals
- Keep easy to prepare/convenience foods around for quick access
Thick Saliva
- Milk, milk products and chocolate can thicken saliva secretions. Try substituting soy products in place of regular milk, ice cream and yogurt.
- Ensure adequate fluid intake to help thin your saliva.
- Try drinking hot tea with lemon to help thin your secretions.
- If you are experiencing excess saliva production, limit very sour or very sweet foods as these may stimulate your salivary glands.
Vitamins, Minerals and Supplements
There are many questions revolving the use of various vitamins, minerals and supplements for the treatment of ALS. Presently there is no research confirming the beneficial effects of any specific nutrition supplement upon ALS. It is recommended to take a general daily multivitamin that provides 100% of the recommended daily intake (RDI) for most vitamins and minerals. If you have chewing or swallowing problems consider a liquid or chewable multivitamin.
Questions?
You will be able to visit with a registered dietitian at your ALS clinic visits here at UPMC Presbyterian Shadyside Hospital. If you have any diet questions between your scheduled clinic visits you can call the dietitian office at 412-647-7999.
Timing of PEG placement
We recommend placement of a PEG in patients who have a significant decline in breathing function whether or not they are having difficulty swallowing, because it becomes more difficult to tolerate the procedure if breathing is significantly impaired. We use breathing testing (spirometry) as a guide and recommend placement of PEG before one measure (the forced vital capacity) reaches 50%. If breathing is not significantly impaired, we generally recommend placement of PEG when patients are losing weight that they are unable to maintain with oral intake or if they have obvious significant swallowing problems that will likely soon lead to loss of weight.
Maintaining Proper Nutrition by Tube Feeding

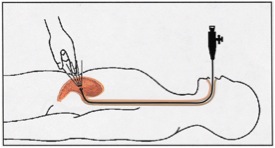
Despite all efforts, patients may lose the ability to eat as a result of the increased time required to eat or from more frequent episodes of coughing or choking. As intake by mouth becomes difficult and often insufficient, alternative methods of feeding should be considered. The device used most often is the percutaneous endoscopic gastrostomy (PEG) tube. PEG tubes are available in the “tube” (pictured on the left) or “button.” The PEG tube should be placed by an experienced gastroenterologist or surgeon through an endoscope (above right). This usually requires and overnight admission in the hospital. During the procedure, a physician puts a tube with a light down your esophagus and into your stomach. The light shines through the abdominal wall to help the doctor find the right spot to place the tube. A small incision will be made in the abdominal wall where the tube will be inserted. The patient or family will be instructed on the use of the PEG in the hospital and should be followed by the family doctor or gastroenterologist. Patients who have a PEG are still able to eat by mouth as long as they are able to swallow safely. Later a Mickey button can replace the tube.

By,
Kathy Zatavekas, MBA, RD, LDN
